Myopia is a significant public health problem in China. High myopia significantly increases the risk of irreversible vision impairment, imposing a substantial medical burden. Consequently, myopia has long received high-level national attention. In August 2018, eight departments, including the Ministry of Education and the National Health Commission, issued the Implementation Plan for Comprehensive Prevention and Control of Myopia in Children and Adolescents. This plan incorporated myopia prevention and control into government performance evaluations as mandatory targets, clearly defining the direction and requirements for myopia control efforts. In recent years, with the implementation of these policies, societal awareness of myopia has significantly increased, and the importance of myopia prevention has become widely recognized. Parents, schools, and society have gained a clearer understanding of the dangers of myopia and generally hope to adopt earlier and more proactive measures to prevent its onset.
Research Background
In October of last year, the Ministry of Education, in conjunction with the National Health Commission and the National Disease Control and Prevention Administration, jointly issued the Notice on Effectively Securing the Key Stages of Myopia Prevention and Control in Kindergartens and Primary Schools. This notice proposed "shifting the intervention focus earlier, securing the key stages of myopia prevention and control in kindergartens and primary schools, and effectively reducing the incidence of myopia among preschool and primary school children," explicitly identifying "shifting the intervention focus earlier" as the priority for future myopia control work.
At the academic level, researchers have also focused on the "pre-myopia" group – children who are not yet myopic but are highly likely to develop myopia in the near term. Interventions such as low-dose atropine, low-intensity red light therapy, and myopia-control spectacles have shown efficacy in this population. However, not all non-myopic children will develop myopia, and over-intervention may cause side effects. Therefore, accurately identifying non-myopic children who truly require intervention and providing early intervention is key to achieving precise myopia control and enabling the "shift of the intervention focus earlier."
Most existing studies rely on baseline characteristics, such as refractive error, axial length, corneal curvature, and axial length-to-corneal radius ratio (AL/CR ratio), with less consideration given to dynamic features of myopia progression, such as the myopic shift over the previous year.
To address this, Professor Yang Xiao's team from the Zhongshan Ophthalmic Center (ZOC) at Sun Yat-sen University, collaborating with Professor Lu Ciyong's team from the School of Public Health at Sun Yat-sen University, conducted a 5-year prospective cohort study covering 12 primary schools in Guangzhou. By combining cycloplegic refraction data and historical axial elongation data, they successfully developed a myopia onset prediction model, proposed a set of criteria for defining "pre-myopia," and created an online myopia onset risk calculator. This achievement holds promise for enabling early warning of myopia onset, improving the precision of myopia interventions, and empowering the "shift of the intervention focus earlier" in myopia control.
Study Details
1. Predictive Value of Baseline Refraction/Axial Length and Historical Changes
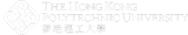
To evaluate and compare the predictive power of historical changes in refraction/axial length versus baseline refraction/axial length, the study first used the third follow-up as the analysis baseline (Fig 1A). Changes in axial length and refraction over the preceding 1 and 2 years were traced. Comparisons revealed:
- For Refraction: Baseline refractive error demonstrated significantly higher predictive power for myopia onset than its historical change values (AUC=0.879), whether considering 1-year (AUC=0.670) or 2-year changes (AUC=0.588) (Fig 1B).
- For Axial Length: The change in axial length over the preceding 1 year showed significantly better predictive power (AUC=0.806) than baseline axial length (AUC=0.696), and also outperformed the change over the preceding 2 years (AUC=0.675). These results were confirmed in the validation cohort.
Fig 1: Comparison of the predictive value of historical refraction and axial length changes for subsequent myopia onset.
2. Establishment and Performance Evaluation of the Myopia Onset Prediction Model
Since incorporating 2 years of historical data offered limited improvement in model performance, the final model was built using baseline refraction combined only with the preceding 1 year of data. Specifically, the second follow-up was used as the analysis baseline to predict myopia onset over the subsequent 1 to 4 years (Fig 2). The model demonstrated good predictive performance, maintaining high efficacy even for prediction at year 4 (AUC=0.879, main cohort; AUC=0.877, validation cohort). The model showed good calibration (Brier scores all <0.25), and Decision Curve Analysis (DCA) indicated clinical utility across various risk thresholds. The team has made this model publicly available as an open-source, free online calculator: https://zoc-qgzk.github.io/pre-myopia-calculator
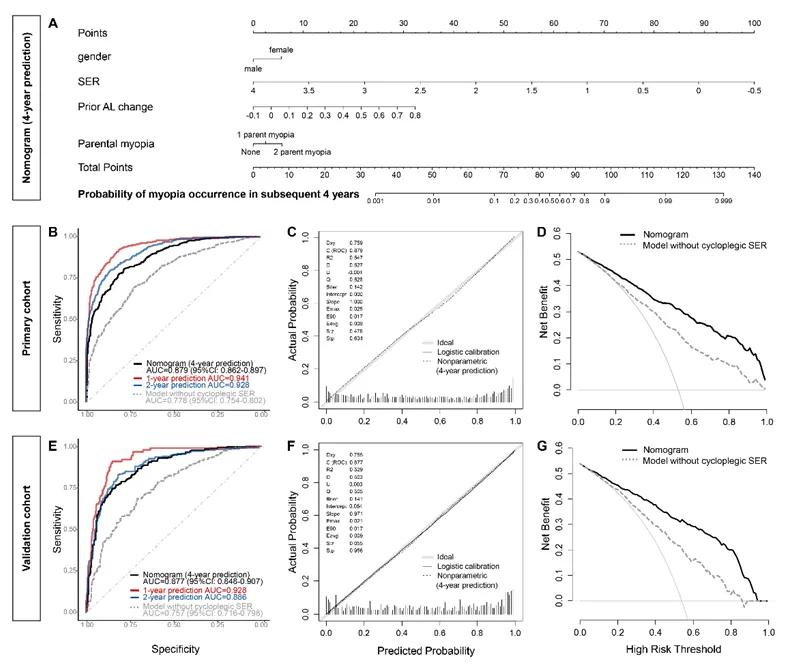
Fig 2: Myopia onset prediction model for subsequent 4 years, established using baseline refraction combined with axial progression over the preceding 1 year.
3. Establishing "Pre-Myopia" Criteria Based on the Model
Previous criteria for defining "pre-myopia" relied solely on hyperopic reserve (e.g., using thresholds like +0.50D or +0.75D), assuming this group would progress to myopia in the short term. However, this standard is overly simplistic, failing to account for individual age and historical myopic shift. For instance: two children both with a hyperopic reserve of +1.00D, but with axial elongation of 0.4mm vs. 0.1mm over the previous year, clearly have different future myopia risks.
This study comprehensively considered factors including refractive error, historical axial elongation, age, and parental myopia, creating detailed risk distribution charts for hyperopic reserve (Fig 3). It was found that greater historical axial progression and longer prediction horizons require a larger hyperopic reserve to indicate low risk.
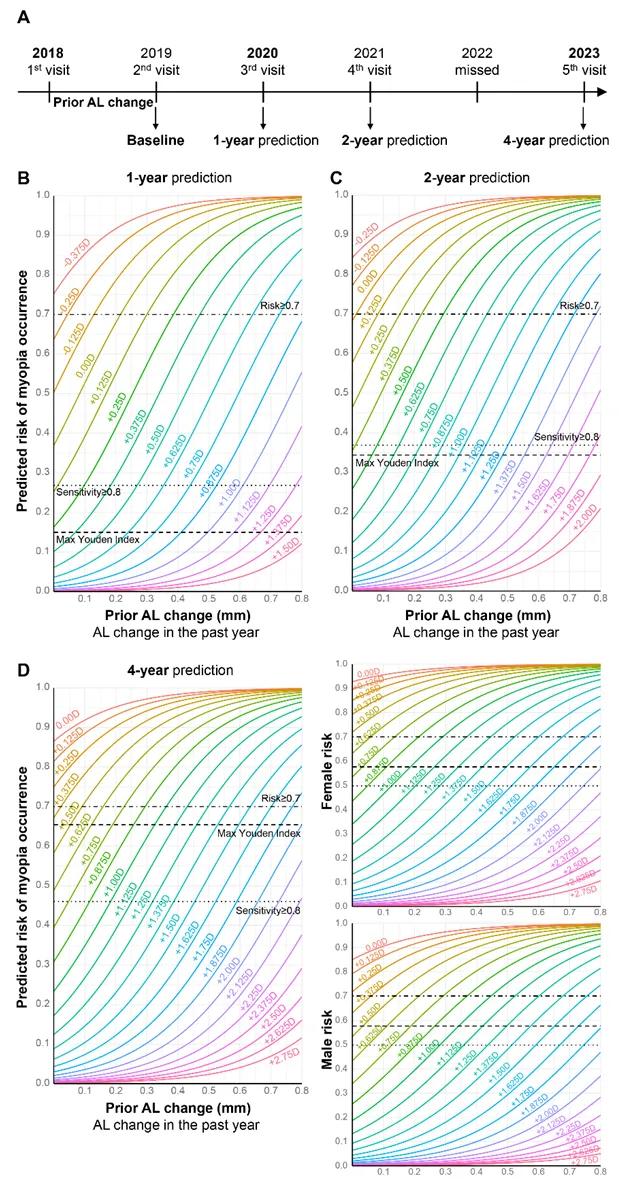
Fig 3: Risk Distribution Chart for Hyperopic Reserve
In summary, based on this 5-year prospective cohort study covering 12 primary schools in Guangzhou, the team, for the first time, combined cycloplegic refraction with historical axial elongation data to establish and validate a myopia onset prediction model. They also proposed a set of criteria for defining "pre-myopia" and developed an online myopia onset risk calculator (https://zoc-qgzk.github.io/pre-myopia-calculator). This achievement holds promise for enabling early warning of myopia onset, improving the precision of myopia interventions, and empowering the "shift of the intervention focus earlier" in myopia control. In the future, the team plans to build upon this work to develop prediction models for myopia progression in already myopic individuals, covering the entire myopia development process.
The above results were published online on June 16, 2025, in the authoritative ophthalmology journal Ophthalmology. Professor Yang Xiao from the Zhongshan Ophthalmic Center, Sun Yat-sen University, is the corresponding author. Professor Lu Ciyong from the School of Public Health, Sun Yat-sen University, and Associate Chief Physician Hu Yin from the Zhongshan Ophthalmic Center are co-corresponding authors. Xu Shengsong (Professional Doctoral Candidate, ZOC), Ruan Zhenbang (MD-PhD Candidate [8-year program], ZOC), and Wang Yanbin (Undergraduate Student [8-year program], Zhongshan School of Medicine) are co-first authors.
Link to Original Article:
https://www.aaojournal.org/article/S0161-6420(25)00359-8/abstract
DOI: 10.1016/j.ophtha.2025.06.010
Research Team
01 Corresponding Authors

Yang Xiao, Professor
Zhongshan Ophthalmic Center, Sun Yat-sen University

Lu Ciyong, Professor
School of Public Health, Sun Yat-sen University

Hu Yin, Associate Chief Physician
Zhongshan Ophthalmic Center, Sun Yat-sen University
02 First Authors

Xu Shengsong
Professional Doctoral Candidate
Zhongshan Ophthalmic Center, Sun Yat-sen University

Ruan Zhenbang
MD-PhD Candidate (8-year program)
Zhongshan Ophthalmic Center, Sun Yat-sen University
Wang Yanbin
Undergraduate Student (8-year program)
Zhongshan School of Medicine, Sun Yat-sen University